
COVID-19 Mortality Rate Declines Significantly in Sweden
Dr. Ananya Mandal, MD via News-Medical Net – A new observational study by Swedish researchers shows a significant decline in death rates among hospitalized patients infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Their study titled, “Decline in mortality among hospitalized covid-19 patients in Sweden: a nationwide observational study,” was released online as a preprint on the medRxiv* server.
Background
The novel coronavirus SARS CoV-2 that causes coronavirus disease (COVID-19), has infected over 44 million individuals worldwide and claimed the lives of over 1.17 million. Most COVID cases are hospitalized for complications caused by the infection.
The virus’s immense capacity to infect populations and spread rapidly has put enormous pressure on the healthcare system in general and on hospitals in particular, wrote the researchers. Those admitted to hospitals with COVID have a mortality of over 20 percent. Thirty-four percent of patients require intensive care. The proportion of patients requiring ICU admission is between 17 and 32 percent wrote the team. These numbers are derived from studies conducted between February and April 2020. With time, the understanding of the infection and its management has improved, and thus survival has also improved with time.
This new study was undertaken among Swedish patients to see if there has been a change in mortality rates among hospitalized COVID-19 patients across the nation. The researchers attempted to see 60-day mortality (defined as death from any cause within 60 days of index hospital admission), mortality rate of the COVID-19 patients for both non-ICU treated, and ICU treated patients during the first 4 months of the pandemic. The data came from the Swedish National Board of Health and Welfare (NBHW).
Study design
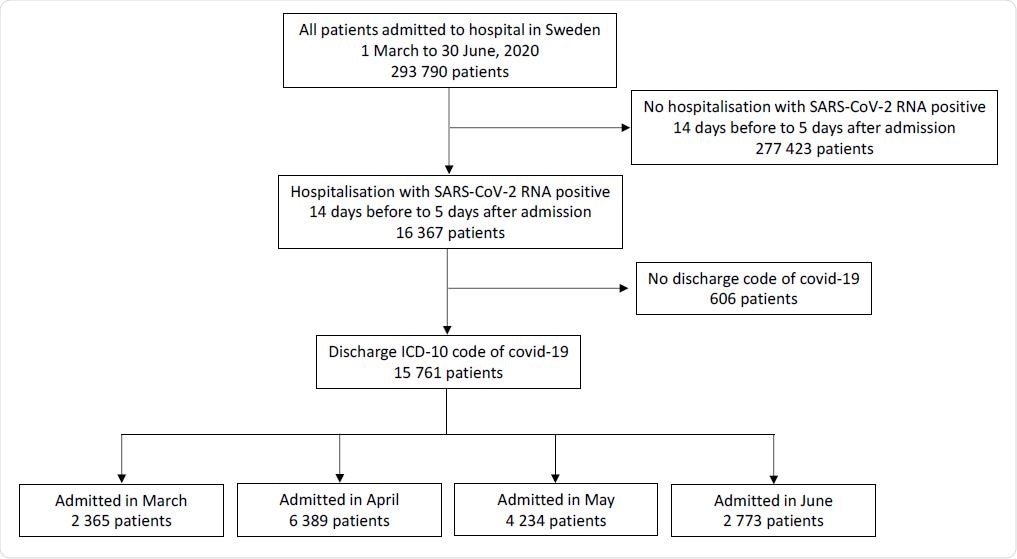
This was a nationwide observational cohort study of patients hospitalized in Sweden between 1st March and 30th June 2020. The patients had all tested positive for SARS-CoV-2 RNA between 14 days before to 5 days after admission. The code on their discharge was COVID-19. All hospitals in Sweden were included in the study.
A total of 15,761 hospitalized patients with COVID-19 were included in the study. The data came from the Swedish National Board of Health and Welfare. 60-day all-cause mortality for the patients was recorded and analyzed. The patient population was classified according to the month of their admission. Relative risks of deaths in the patients by month of admission were calculated. Factors such as pre-existing comorbidities, age, gender and care dependency, and severe illness were considered.
To assess the severity of illness, Simplified Acute Physiology, version 3 (SAPS3), and oxygenation index (PaO2/FiO2) were used among ICU admitted patients. Treatments and procedures they underwent in the ICU were also recorded.
What was found?
Overall results of the study can be summarized as:
- A total of 15,761 patients were admitted.
- The patients’ median age was 64 years (between 51 and 78 years), and of these, 57.5 percent were men.
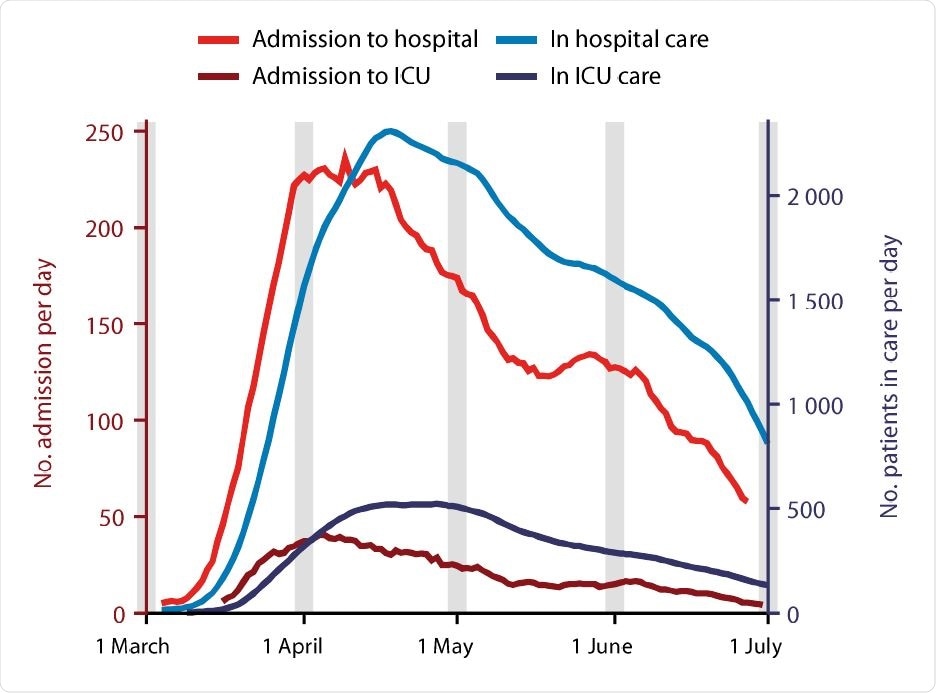
- The highest number of admissions was during April 2020
- The proportion of patients admitted to ICU was 14.4 percent overall.
- Age distribution of admitted patients changed over time, with the number of patients less than 40 years old and over 90 years of age rising between March and June.
- The overall all-cause 60-day mortality was 17.8 percent (between 17.2 and 18.4 percent) among Swedish patients hospitalized with COVID-19.
- The rates of deaths were 24.7 in March 2020 that fell to 13.3 percent in June 2020
- Adjusted relative risk (RR) of death was 0.56 (95 percent CI, 0.51 to 0.63) for June, with rates inMarch used as a baseline.
- Compared to ICU admitted patients, relative risks of death for non-ICU patients were 0.60 (95 percent CI, 0.53 to 0.67) and 0.61 (95 percent CI, 0.48 to 0.79), respectively.
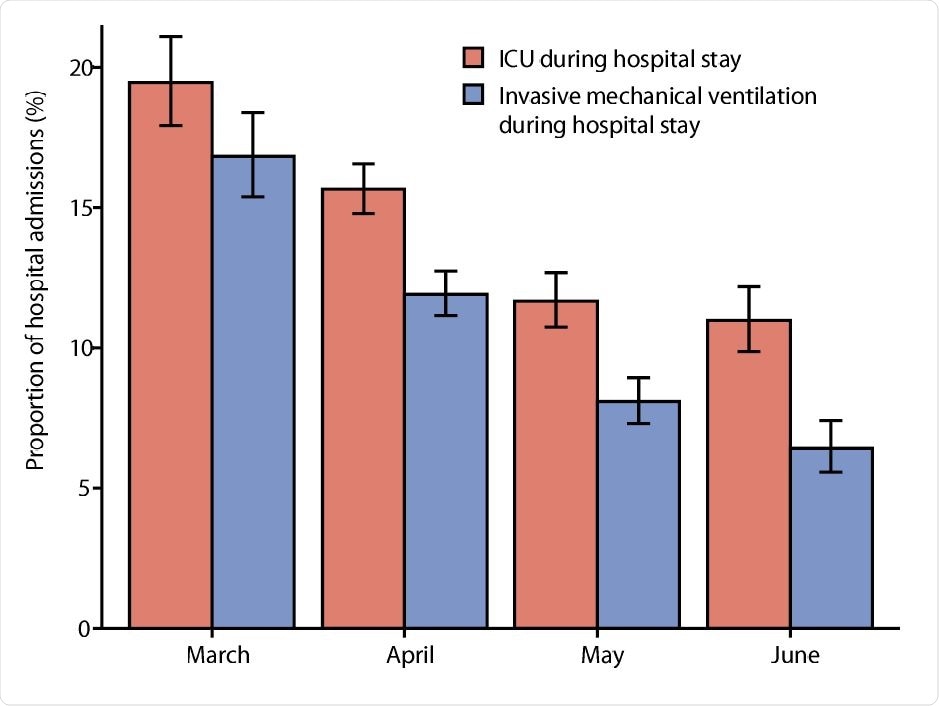
- Admission rates to the ICU fell from 19.5 percent (95 percent CI, 17.9 percent to 21.0 percent) in March to 11.0 percent (95 percent CI, 9.9 percent to 12.2 percent) in June 2020.
- In June, the proportion of ICU admitted patients receiving mechanical ventilation fell from 86.5 percent in March to 58.6 percent.
- In June, the proportion of ICU admitted patients receiving dialysis fell from 22.8 percent in March to 13.8 percent.
- SAPS3 and PaO2/FiO2 on ICU admission remained similar throughout the study period among the patients
Conclusions and implications
This study reveals that there has been a decline in the mortality rates among hospitalized Swedish COVID-19 patients with time over the pandemic. This decline is independent of the pre-existing comorbidities among the patients. Authors call for further research to understand the reasons behind this decline. Authors write, “The changing covid-19 mortality should be taken into account when management and results of studies from the first pandemic wave are evaluated.”
*Important Notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Decline in mortality among hospitalised covid-19 patients in Sweden: a nationwide observational study Kristoffer Stralin, Erik Wahlstrom, Sten Walther, Mona Heurgren, Anna M Bennet-Bark, Thomas Linden, Johanna Holm, Hakan Hanberger medRxiv 2020.10.27.20220061; doi: https://doi.org/10.1101/2020.10.27.20220061, https://www.medrxiv.org/content/10.1101/2020.10.27.20220061v1
To read the original article click here.






